Resident physician receives scholarship to care for patients in Haiti
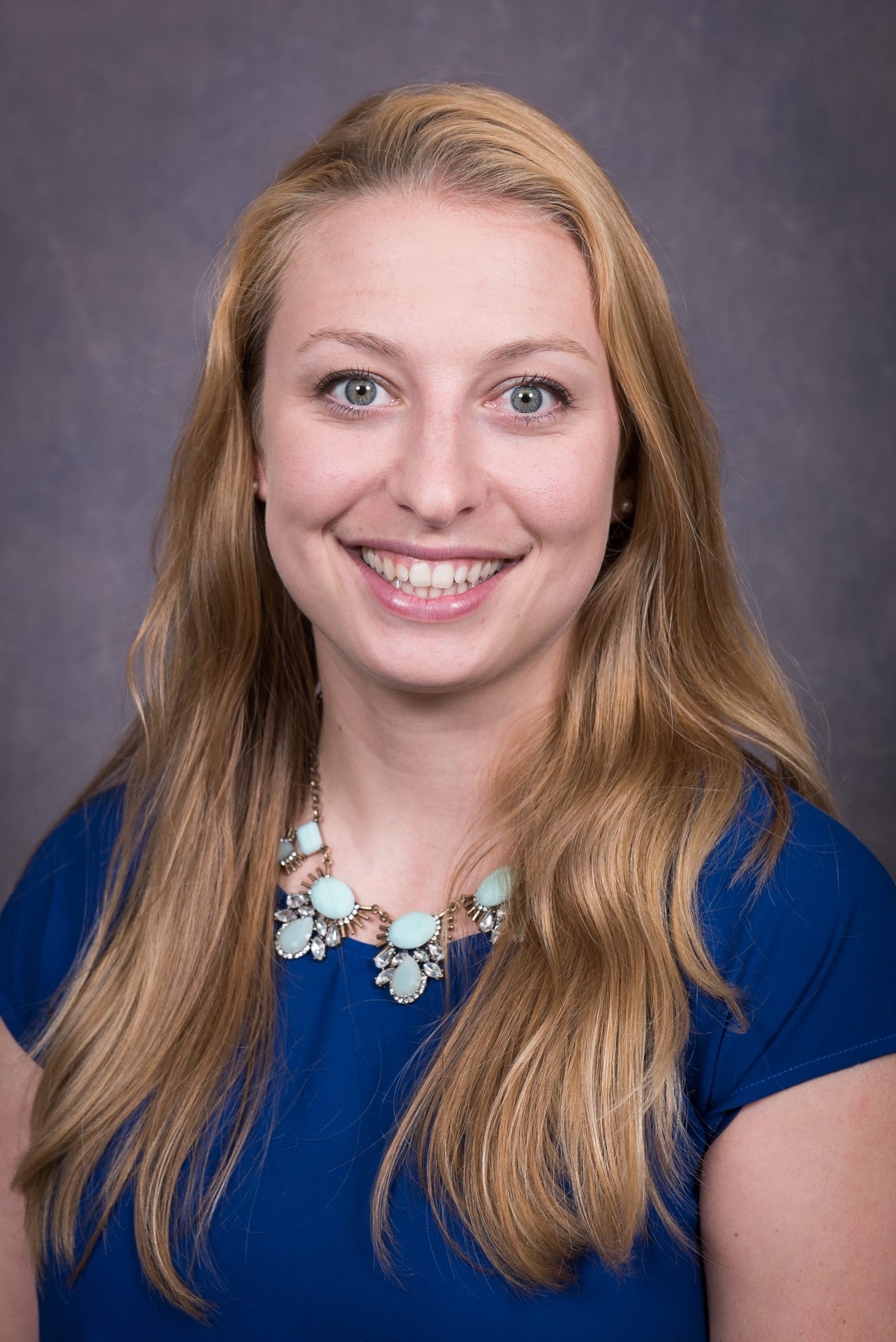
Dr. Natalie Kuijpers, a chief resident of The University of Alabama Family Medicine Residency, has received a scholarship to provide patient care in Haiti. The residency is operated by the College of Community Health Sciences. Kuijpers is one of only two family medicine residents in the US to receive the scholarship, which is awarded by…